A currently available pill could significantly curb new HIV infections among gay and bisexual men in the UK, if prevention and treatment programs are also expanded, researchers say.
Wider use of the once-a-day pill, along with HIV blood tests and treatment among very sexually active men who have sex with men, could potentially reduce new cases by about 44 percent by 2020, researchers say.
The new research shows that "combination approaches, even if implemented among only a targeted or limited population, can have a larger impact than single interventions alone," said Dr. Jason Kessler, an HIV researcher who was not involved with the new study.
Of the more than 100,000 UK residents with HIV infections in 2014, about 43 percent were gay or bisexual men, the authors of the study write in The Lancet HIV.
In this population, attempts to reduce transmission of the AIDS-causing virus by focusing on condom use and frequent blood tests have been ineffective, the authors say.
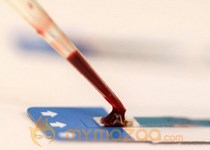
A new Gilead drug marketed as Truvada (containing tenofovir disoproxil and emtricitabine) has emerged as another prevention strategy.
Rather than waiting to catch the virus, people take Truvada before they get infected. Truvada is thought to cut the risk of sexually-transmitted HIV by 90 percent.
This practice of treating people with medicine to prevent them from catching a communicable disease is known as PrEP, which stands for "pre-exposure prophylaxis."
For the new study, Narat Punyacharoensin of the London School of Hygiene and Tropical Medicine and colleagues used computers to estimate the number of new HIV cases among gay and bisexual men in the UK by 2020 and then to predict how different prevention methods might change the number of infections.
They estimated that nearly 17,000 gay and bisexual men ages 15 to 64 would become newly infected with HIV between 2014 and 2020.
By itself, expanding PrEP to all gay and bisexual men in the UK would prevent about 59 percent of infections, the computer model estimates. Even just targeting those at highest risk of HIV infection with PrEP would still reduce infections by more than half.
A large percentage of HIV infections could also be prevented if the only thing gay and bisexual men did was to reduce the number of repeat sexual partners or decreased unprotected sex with repeat sexual partners, the researchers say.
But even if PrEP - combined with yearly HIV testing and a test-and-treat program - were used only by the men in the top 25 percent for sexual activity, more than 7,000 new cases could be prevented by 2020, they estimate.
Compared to treating every gay and bisexual man in the UK, targeting the most sexually active people is feasible, according the researchers.
Kessler, of NYU Langone Medical Center in New York City, believes that prioritizing PrEP "among those at particularly 'high-risk' would be the most efficient method of implementation."
However, he told Reuters Health by email, PrEP is not widely used right now.
"I think that the practical or conservative scenarios the authors of this article suggest are potentially achievable in the next 5-10 years . . . in jurisdictions that 'buy-in' to the use of PrEP as a HIV prevention tool," he said.
In the U.S., Truvada costs approximately $1,500 a month. Some insurance plans cover it; financial assistance programs are also available.