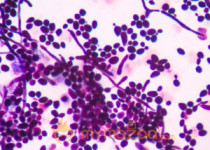
Researchers from Johns Hopkins University have observed a link between yeast infections and a history of mental illness. In their study, published Wednesday in the journal npj Schizophrenia, the authors caution that the association doesn’t prove a causal effect but that it may provide insight on how lifestyle, immune system weaknesses and gut-brain connections may affect an individual’s risk of psychiatric disorders and memory impairment.
Prompted by suggestions from people with mental illness and previous findings that suggested a link, researchers found that Candida yeast infections were more common in a group of men with schizophrenia or bipolar disorder than in men without those disorders. Among women with schizophrenia or bipolar disorder, researchers found that those who tested positive for Candida did worse on a standard memory test than those who didn’t have a history of the infection or diagnoses of the disorders.
“It’s far too early to single out Candida infection as a cause of mental illness or vice-versa,” Emily Severance, assistant professor of pediatrics and member of the Stanley Division of Developmental Neurovirology at the Johns Hopkins University School of Medicine, said in a news release. “However, most Candida infections can be treated in their early stages, and clinicians should make it a point to look out for these infections in their patients with mental illness.”
Severance and her team studied the relationship between Candida and mental illness after receiving patient testimonials, and learning that previous research linked schizophrenia with immune system problems— and weakened immune systems make individuals more susceptible to fungal infections.
To examine the potential association, researchers at the Sheppard Pratt Health System took blood samples from about 800 people ages 18 to 65. About 280 had no history of mental disorder, about 260 had schizophrenia and 270 had bipolar disorder. Study authors looked for the presence of IgG class antibodies to Candida, which indicates a history of yeast infection. They then analyzed their results for associations between mental illness and history of yeast infection.
When looking at the study group as a whole or at the women alone, researchers didn’t identify a link between the presence of Candida antibodies and an increased risk of mental illness. But among the male group, study authors observed that 26 percent of those with schizophrenia had a history of the infection, compared with 14 percent of the control males. They also found that, among the men, those with bipolar disorder had about a 26 percent yeast infection rate compared to only 14 percent in the male control group.
To study whether a history of yeast infection could have an effect on neurological responses, participants completed a 30-minute cognitive test to assess immediate memory, delayed memory, attention skills, use of language and visual-spatial skills, according to the release.
Using a 100-point scale, researchers found the control men and women with and without a history of yeast infection had no measurable differences in scores in the five neurological responses. But the women with schizophrenia and bipolar disorder who also had a history of the infection scored lower on the memory portions of the test than those who had no history of infection.